Back pain from epidural can affect up to 31% of patients years after the procedure. This happens even to patients who never had back issues before. These numbers tell a surprising story about a medical procedure many people call routine.
Every year, around 100,000 women in Britain receive epidural anesthesia to manage labor pain. While this brings vital pain relief, we need to think about what it means long-term. Patients might experience lasting back pain due to nerve damage, infection, or spinal cord injury during the procedure. A randomized study of 369 women revealed something interesting – the chances of developing long-term back pain were similar whether women had epidurals or not. This suggests that pregnancy and childbirth themselves might play an equally important role in causing discomfort.
Relief starts with understanding why back pain happens after epidurals. Most women feel better within a week after delivery. Some discomfort can last up to six weeks, and certain cases might take even longer to resolve. This piece explores natural remedies and lifestyle changes that help. It also points out warning signs that tell you when it’s time to see a doctor about persistent lower back pain after an epidural.
Table of Contents
- 1 Understanding Epidural and Its Effects on the Back
- 2 Why Lower Back Pain May Persist After an Epidural
- 3 Natural Remedies to Ease Persistent Back Pain
- 4 When to Seek Medical Help for Post-Epidural Pain
- 5 Lifestyle Changes to Support Long-Term Recovery
- 6 Here are some FAQs about lower back pain from epidural years later:
- 6.1 Does an epidural affect you later in life?
- 6.2 How do you know if an epidural messed up your back?
- 6.3 What are the symptoms of nerve damage from an epidural?
- 6.4 How to treat back pain from epidural?
- 6.5 Why does my back hurt 4 years after an epidural?
- 6.6 How many times can you get an epidural in your life?
- 6.7 Can an epidural cause sciatica?
- 6.8 Can you sue for back pain after an epidural?
- 6.9 What are the long-term side effects of spinal anaesthetic?
 Understanding Epidural and Its Effects on the Back
Understanding Epidural and Its Effects on the Back
An epidural is a special injection that delivers medication right into the space around the spinal cord. Doctors have used epidural anesthesia as a pain control method for more than 100 years. This technique works better than many other types of anesthesia. The numbers show how popular it is – about 100,000 women in Britain get epidurals during childbirth each year.
What happens during an epidural procedure
The patient starts by either sitting and leaning forward or lying on their side with knees pulled close to the chest. A healthcare professional numbs the skin with a local anesthetic where they’ll insert the epidural. Then an anesthetist uses a needle to place a thin plastic tube (catheter) near the spinal nerves that send pain signals to the brain.
The doctor removes the needle once the catheter is in place. They then send medication through this catheter – usually local anesthetics or steroids based on what’s needed. These medications temporarily numb the spinal nerves and block pain signals from reaching specific body areas.
Patients stay awake during the procedure but might feel mild discomfort or pressure when the doctor positions the needle and inserts the catheter. Pain relief kicks in within 10-20 minutes. The catheter often stays in place for several hours or even days for childbirth or after surgery. This allows continuous medication delivery.
Common short-term side effects
Epidurals work well but can cause some short-term side effects:
- Localized soreness: The injection site often feels tender, but this goes away in a few days
- Low blood pressure: This affects about 13 out of 100 women and can make them feel dizzy, nauseated, or lightheaded
- Urination difficulties: Around 18 out of 100 women have trouble controlling their bladder because their lower body feels numb
- Fever: About 15 out of 100 women with epidurals get fever, compared to just 6 out of 100 who choose other pain treatments
- Itching: This bothers roughly 3 out of 100 women
On top of that, bad headaches can happen if the epidural needle accidentally punctures the protective membrane (dura mater) around the spinal cord. This leads to cerebrospinal fluid leakage in about 1-2% of cases.
Why some people experience pain years later
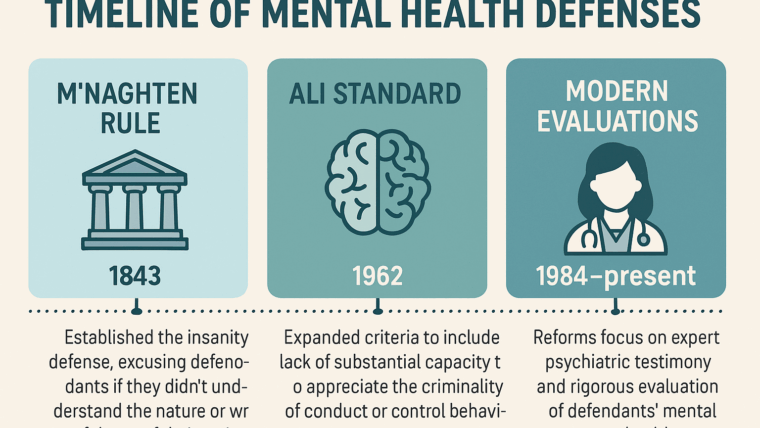
Scientists have done lots of research on the connection between epidurals and long-term back pain. The results aren’t clear-cut. While temporary discomfort happens often, permanent back problems from epidurals are quite rare.
In spite of that, some studies looking back at patient histories have found possible links between epidurals and ongoing discomfort. MacArthur and colleagues found an unexpected connection between epidural pain relief during labor and back pain that lasted more than three months. This held true even after they ruled out other factors. Russell’s team found that 18% of women who got epidural analgesia had long-term back pain, while only 12% of women using other pain relief methods experienced this.
But newer controlled studies tell a different story. One study that followed patients over time found no real difference in back pain between women who got epidurals and those who didn’t.
Back pain is nowhere near unusual for new mothers, whether they had an epidural or not. About two-thirds of young mothers say they have back pain up to two years after giving birth. Many of these women had back pain before getting pregnant, which suggests other things besides epidurals cause most postpartum back discomfort.
Why Lower Back Pain May Persist After an Epidural
Patients can experience ongoing discomfort after epidural procedures through several mechanisms. These problems might develop months or years after the original procedure. Understanding these mechanisms helps patients find the right treatment approaches that work best for them.
Nerve irritation or damage
Lasting pain often stems from direct trauma to nerve tissue. The epidural needle or catheter can damage a single nerve, multiple nerves, or rarely, the spinal cord itself. Patients demonstrate numbness, pins and needles sensations, or weakness in specific body areas. On top of that, nerve compression can happen from blood collection (hematoma) near the nerve roots, especially in patients who have coagulation disorders.
Nerve damage can be temporary or permanent. Most patients with mild nerve damage recover fully within days to weeks, though some cases need several months. This is a big deal as it means that severe cases can lead to permanent loss of feeling or movement, though this happens in only 1 in 23,500 to 1 in 50,500 spinal or epidural injections.
Injection site trauma
Trauma at the injection site can trigger aseptic inflammation of subcutaneous tissues. Patients sometimes come back days after the procedure with new-onset atypical back pain that doesn’t follow a clear dermatomal pattern. The inflammation shows up as severe pain at the needle entry site and can spread to surrounding areas.
Antiseptic solutions like chlorhexidine—used during the procedure—might not dry completely before administration. This allows cytotoxic chemicals to enter tissues and cause inflammation. Such reactions usually clear up with conservative management within several days.

Pre-existing spinal conditions
Pre-existing spinal pathologies increase the risk of complications. Spinal stenosis (narrowing of the spinal canal) or compressive lumbar disk disease leaves less anatomic space for fluid collections. Even small amounts of injected fluid can increase pressure around neural structures and potentially worsen symptoms.
Undiagnosed spinal issues might become obvious after an epidural. Some patients have dormant pre-existing neurological conditions that only show up after the functional changes caused by the procedure.
Posture and labor positioning
Labor positions affect pelvic dimensions and spinal alignment. The mother’s position changes alter her pelvis’s spatial shape, which affects how the fetus adapts to the labor canal. Poor positioning during labor with an epidural might lead to lasting structural changes.
Research shows that lying on your back specifically lowers blood pressure, increases low back pain, and slows labor progress. Standing positions help with spontaneous pushing, improve uterine contractions, and speed up fetal head descent.
Inflammation or scar tissue formation
Epidural fibrosis—scar tissue formation in the epidural space—might be the biggest factor in long-term pain. This fibrotic adhesion develops from local trauma and inflammation. The scar tissue’s main harmful effect comes from compressing the neural microvasculature, which leads to ischemic injury.
Epidural fibrosis affects up to 30% of patients after lumbar procedures and makes persistent low back pain 3.2 times more likely. The scar tissue forms slowly, which explains why some patients feel better right after an epidural but start having pain again about six weeks later.
Moving around each day causes nerval structures to shift, which often triggers and worsens pain in patients with epidural fibrosis. Bending the spine puts more mechanical stress on scar-adhered nerve structures, which adds to chronic discomfort.
Natural Remedies to Ease Persistent Back Pain
Natural approaches are a great way to get relief from lower back pain caused by past epidural procedures. These non-drug strategies help manage ongoing discomfort without medication side effects.
Gentle stretching and yoga
Yoga helps soothe lower back pain better than most treatments. This ancient practice strengthens vital supporting muscles like paraspinal muscles that help bend the spine, multifidus muscles that keep vertebrae stable, and the transverse abdominis that supports the spine. Cat-cow poses work the erector spinae and rectus abdominis muscles. Child’s pose gently stretches the gluteus maximus and spinal extensors. Research shows yoga works just as well as physical therapy for chronic lower back pain. This holds true even for low-income, minority patients who might not have easy access to treatment.
Heat and cold therapy
Temperature changes can affect back pain recovery by a lot. Heat therapy triggers thermoreceptors that block pain signals in the lumbar dorsal fascia and spinal cord. Just a 1°C rise in tissue temperature boosts local metabolism by 10-15%. This leads to better blood flow and faster healing. Cold therapy reduces blood flow and slows metabolic processes, which helps decrease inflammation and swelling. The best results come from applying ice wrapped in a towel for 10-15 minutes during acute pain (within 6 hours). After that, switch to heat therapy for longer relief.
Massage and myofascial release
Myofascial release therapy helps relieve pain by applying gentle, steady pressure to tight spots or “trigger points” in connective tissues. This method works well for people with chronic back pain. Studies show notable improvements in back disability scores (SMD = −0.35) for patients who got myofascial treatment. Sessions usually last 15-50 minutes, and patients should get treatments every one to three days.
Herbal anti-inflammatories
Natural compounds reduce inflammation without the side effects of regular drugs. Some effective options include:
- Turmeric (containing curcumin)
- Omega-3 essential fatty acids
- Devil’s claw (containing harpagoside)
- Boswellia serrata (Indian frankincense)
- Green tea (containing EGCG)
Research shows these natural compounds work like NSAIDs to block inflammatory pathways.
Mind-body techniques like meditation
Mindfulness-based methods teach you to pay attention to present experiences without judgment. These techniques change how you relate to pain instead of trying to change the pain itself. This helps separate physical sensations from suffering. The body scan technique works well for pain conditions. By observing discomfort without judgment, you can help your body relax even when pain continues.
When to Seek Medical Help for Post-Epidural Pain
Knowing how to spot signs that require professional medical help after epidural pain is vital to prevent serious complications. Most side effects from epidurals go away on their own, but some symptoms need immediate medical evaluation.
Signs of nerve damage or infection
Nerve damage doesn’t happen often but needs quick intervention. Look out for numbness or tingling sensations in your legs or lower body that come with unusual painful sensations. Your muscles might also become weak in one or more groups, which could point to nerve problems.
Signs of infection need urgent medical care. Your symptoms might include fever, back pain that gets worse, or changes in consciousness – these could mean you have an epidural abscess, which needs treatment right away. These infections can develop near your spinal cord and major nerves and might cause permanent damage if you don’t get help.
Pain that worsens over time
You should see a doctor if your pain gets worse instead of better in the days or weeks after an epidural. The injection site often feels sore at first, but pain that doesn’t go away or gets worse might show a deeper problem.
Research shows that regular postpartum back pain usually goes away within six months after delivery. Pain that lasts longer than this, especially with other symptoms, needs a doctor’s evaluation.
Loss of mobility or bladder control
Loss of mobility or bladder control ranks among the most serious warning signs that need emergency care. You should worry if you have trouble controlling your bowel or bladder functions after the epidural wears off because it might show spinal cord problems. Call emergency services right away if you notice:
- Sudden leg weakness or paralysis
- Problems walking or moving around
- Loss of bowel or bladder control
- Can’t empty your bladder
Spinal epidural abscesses don’t happen often (0.2-2.8 cases per 10,000 hospital admissions). Only 10-15% of patients show the classic three signs – back pain, fever, and declining neurological function – during their first visit. The window to treat severe cases effectively becomes very small once neurological problems start, with just 8 hours to perform surgery in the worst cases.
Lifestyle Changes to Support Long-Term Recovery
Getting better from stubborn lower back pain after an epidural needs lifestyle changes that help you heal properly. These smart changes can make a big difference in reducing your discomfort and stopping future pain.
Improving posture and ergonomics
Good posture builds the foundation of a healthy back. Your spine’s natural curve needs protection to cut down muscle strain. Keep your feet flat on the floor with knees at 90-degrees while sitting. Your computer screen should be at eye level to protect your neck from strain that leads to back and neck pain. A workspace with the right furniture, especially chairs that support your lower back, helps keep your spine naturally aligned.
Strengthening core muscles
Your core muscles—including abs, back, and pelvic muscles—give your spine the support it needs. A strong core makes daily activities easier on your back. Simple exercises like bridges help you lift your hips until they line up with your knees and shoulders. Planks work several muscle groups at once, while ab crunches target specific areas. These exercises boost your stability and help prevent injuries.
Avoiding high-impact activities
High-impact workouts can make epidural-related back pain worse. You should try gentler options that raise your heart rate without hurting your spine. Walking is a simple, low-impact exercise that only needs good shoes. You might also try stationary bikes, swimming, or elliptical machines for great cardio that’s easy on your spine. Exercises in water mix resistance with natural floating, which works great for sensitive backs.
Creating a daily movement routine
A steady routine helps you recover better. Take regular movement breaks throughout your day by standing or walking every 30 minutes. Start your morning with stretches to loosen up stiff muscles. Your daily plan should include gentle back stretches—reach up while looking at your hands. Pay attention to what your body tells you, start with 2-3 stretches every hour and add more as you feel stronger.
Back pain that persists after an epidural can feel overwhelming. Understanding why it happens is your first step toward managing it better. This piece explores how epidurals affect your back, why pain might last for years, and practical ways to find relief.
Natural remedies are a great way to get relief for many patients with post-epidural discomfort. A combination of gentle yoga, strategic heat and cold therapy, massage, herbal anti-inflammatories, and mindfulness techniques can reduce pain without medication side effects. These approaches enable patients to actively participate in their recovery.
Your lifestyle changes play a significant role in healing over time. Good posture, ergonomic workspaces, core-strengthening exercises, and low-impact activities help maintain spinal health. Regular movement throughout the day prevents stiffness and helps healing.
You should watch for warning signs that need medical help. Medical attention becomes necessary when pain gets worse, you notice signs of nerve damage or infection, or lose mobility or bladder control. Quick action can prevent lasting damage if serious complications arise.
The link between epidurals and lasting back pain isn’t simple. Studies show different results, but one thing is clear – you have many options for relief whatever caused your pain. Most people get better with proper self-care and lifestyle changes.
Post-epidural back pain isn’t permanent. Think of recovery as a steady process that needs patience and regular effort. Natural remedies, timely medical care, and healthy lifestyle habits create a complete system to manage lasting lower back pain and improve life quality.
Here are some FAQs about lower back pain from epidural years later:
Does an epidural affect you later in life?
For most women, epidurals do not cause long-term effects, but a small percentage may experience persistent issues. Some women report on lower back pain from epidural years later reddit forums that they continue to have discomfort long after their procedure.
How do you know if an epidural messed up your back?
You might suspect an epidural complication if you experience persistent, localized pain at the injection site that doesn’t improve with time. Many discussions on lower back pain from epidural years later reddit threads describe this type of ongoing discomfort as a potential indicator of issues.
What are the symptoms of nerve damage from an epidural?
Symptoms of nerve damage from an epidural can include sharp, shooting pain, numbness, tingling, or muscle weakness in the lower back or legs. These are the types of symptoms that some users describe when sharing experiences about lower back pain from epidural years later reddit communities.
How to treat back pain from epidural?
Treatment for back pain from an epidural may include physical therapy, pain management techniques, and in some cases, medication. Many suggestions for managing this discomfort can be found in discussions about lower back pain from epidural years later reddit where users share what has worked for them.
Why does my back hurt 4 years after an epidural?
Back pain four years after an epidural could be due to scar tissue formation, nerve irritation, or the development of other spinal issues that may or may not be related to the procedure. This is a common concern raised in lower back pain from epidural years later reddit conversations.
How many times can you get an epidural in your life?
There’s no specific limit to how many epidurals a person can receive in their lifetime, though each procedure carries its own risks. This medical question is different from the personal experiences shared about lower back pain from epidural years later reddit forums.
Can an epidural cause sciatica?
While rare, an epidural can potentially cause sciatica-like symptoms if nerve roots are affected during the procedure. Some individuals report such symptoms in threads discussing lower back pain from epidural years later reddit platforms.
Can you sue for back pain after an epidural?
You might have legal grounds to sue if you can prove the back pain resulted from medical negligence or improper technique during the epidural administration. This legal question sometimes appears alongside personal accounts of lower back pain from epidural years later reddit discussions.
What are the long-term side effects of spinal anaesthetic?
Long-term side effects of spinal anesthesia are rare but can include persistent headache, back pain, or nerve damage in some cases. These potential outcomes are sometimes described in posts about lower back pain from epidural years later reddit where users share their experiences.